Aspirin is one of those drugs that has been around forever. It is commonly used as a pain reliever, anti-inflammatory, and as a blood thinner. Surprisingly it may also have benefit in treating COVID.
A paper in Anesthesia and Analgesia published last spring titled, “Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease 2019.”
This was a retrospective, observational study of adult patients admitted to multiple hospitals in the U.S. between March and July 2020, in the early days of COVID. The primary outcome addressed by the researchers from George Washington University was the need for mechanical ventilation, which then, and still now, carries an extremely high chance of never leaving the ICU alive.
This was not a gold standard randomized prospective clinical trial. That would not be feasible in this situation since study patients were already hospitalized and critically ill. Remember in the early days, one needed to be extremely ill before even being admitted to the hospital rather than being sent home until sick enough to return and go straight to the ICU.
But the results were impressive. As reported last week by the Jerusalem Post,
The team investigated more than 400 COVID patients from hospitals across the United States who take aspirin unrelated to their COVID disease, and found that the treatment reduced the risk of several parameters by almost half: reaching mechanical ventilation by 44%, ICU admissions by 43%, and overall in-hospital mortality by 47%.

Why would aspirin be helpful for COVID, a respiratory disease? What if COVID is more than simply a lung disease or pneumonia? COVID is actually thought to be a microvascular disease causing blood clots, as described in the medical journal Circulation,
Although most patients with coronavirus disease 2019 (COVID-19) present with a mild upper respiratory tract infection and then recover, some infected patients develop pneumonia, acute respiratory distress syndrome, multi-organ failure, and death. Clues to the pathogenesis of severe COVID-19 may lie in the systemic inflammation and thrombosis observed in infected patients. We propose that severe COVID-19 is a microvascular disease in which coronavirus infection activates endothelial cells, triggering exocytosis, a rapid vascular response that drives microvascular inflammation and thrombosis.
Note the thrombosis aspect, blood clots forming in the lungs and elsewhere in the body. Aspirin, as a blood thinner, reduces the risk of blood clots, explaining its potential benefit for COVID.
For the same reason, the American Heart Association recommends,
If you have had a heart attack or stroke, your doctor may want you to take a daily low dose of aspirin to help prevent another. Aspirin is part of a well-established treatment plan for patients with a history of heart attack or stroke.
Add the appropriate caveat, which I would echo, “You should not take daily low-dose aspirin on your own without talking to your doctor. The risks and benefits vary for each person.”
How did aspirin get its start? Over 3,500 years ago, willow bark, known as “nature’s aspirin,” was used as a painkiller and anti-pyretic by ancient Egyptians and Greeks, and in a chemical synthesis by a Bayer chemist in 1897.
Aside from pain relief, it was found to have anti-platelet and anti-cancer effects. It’s also on the World Health Organization’s list of essential medicines, along with another familiar drug, ivermectin. The Harvard-based physicians’ health study in the 1980s found that low dose aspirin reduced the risk of heart attack by 44 percent.
A recently published Israeli study found, “Aspirin use is associated with better outcomes among COVID-19 positive patients.” This included lower likelihood of infection, disease duration, and hospital survival. In other words, aspirin works as both a preventative and as a...
Read more HERE

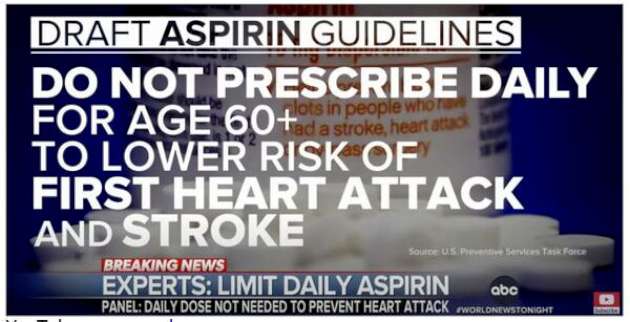
No, aspirin isn't the new "horse dewormer". What is happening here is what has ALWAYS happened, well at least until Covid-19 vaccinations hit the scene. There has always been a "risk-benefit" decision before any treatment, even things as relatively harmless as aspirin. Sure, the younger you are the less likely you are to get a fatal ulcer, but also the less likely you are to benefit for primary heart disease prevention.
ReplyDeletePlease note that if they are saying "don't use under 60" they are committing the same error. There ARE younger people at higher risk for heart disease who can benefit from low dose aspirin as well as people older than 60 who may not.
Imagine that, medicine shouldn't be practiced by "cook book"...
The headache that came with Kung flu delta was almost a migraine. My Dr recommended Tylenol and half way through the dosage time limit to take a BC powder (aspirin). That kept it barely noticeable.
ReplyDeleteI had kung flu 2 months ago and I turn 60 next month. My fully vaxed wife brought it home to me. I had symptoms 2 days after she did.
Massive UK study showed aspirin had no benefit for severely ill patients. Yes it is the new horse dewormer. Useless for Covid!
ReplyDeleteWhat this article doesn't address is "True inflammation" Many fatalities from respiratory complications were due to severe inflammation of the lungs and microvasculature. Any anti-inflammatory (aspirin, steroids, tylenol) would reduce this inflammation and make for a more favorable outcome. Now some in the medical community would shy away from steroids in infectious diseases, BUT if you use anti-inflammatory doses of the drug vs immune suppressive doses, the benefits far outweigh the risks. I believe in this philosophy and because of that, ever since the Rona hit us, I didn't stop my usual "seasonal use" of flonase, an intranasal steroid. I believe it will minimize the inflammation of my respiratory epithelium should I come into contact with the virus. It wouldn't necessarily change the replication of it (like Ivermectin) but would reduce the adverse affects of the virus on the tissues. At least that's where I stand with my immunological training.
ReplyDelete